Diabetes can silently harm your vision by damaging the tiny blood vessels in your eyes, especially in the retina. This damage, called diabetic retinopathy, is the leading cause of blindness in working-age adults. Early stages often show no symptoms, but issues like blurry vision, floaters, or dark spots may eventually appear. Other risks include diabetic macular edema, cataracts, and glaucoma.
The good news? Early detection and treatment can prevent 95% of vision loss. Regular eye exams, managing blood sugar, blood pressure, and cholesterol, and maintaining a healthy lifestyle are essential steps to protect your eyesight. Treatments like anti-VEGF injections, laser therapy, and surgery can address advanced conditions. Don’t wait – schedule an eye exam and take steps to safeguard your vision today.
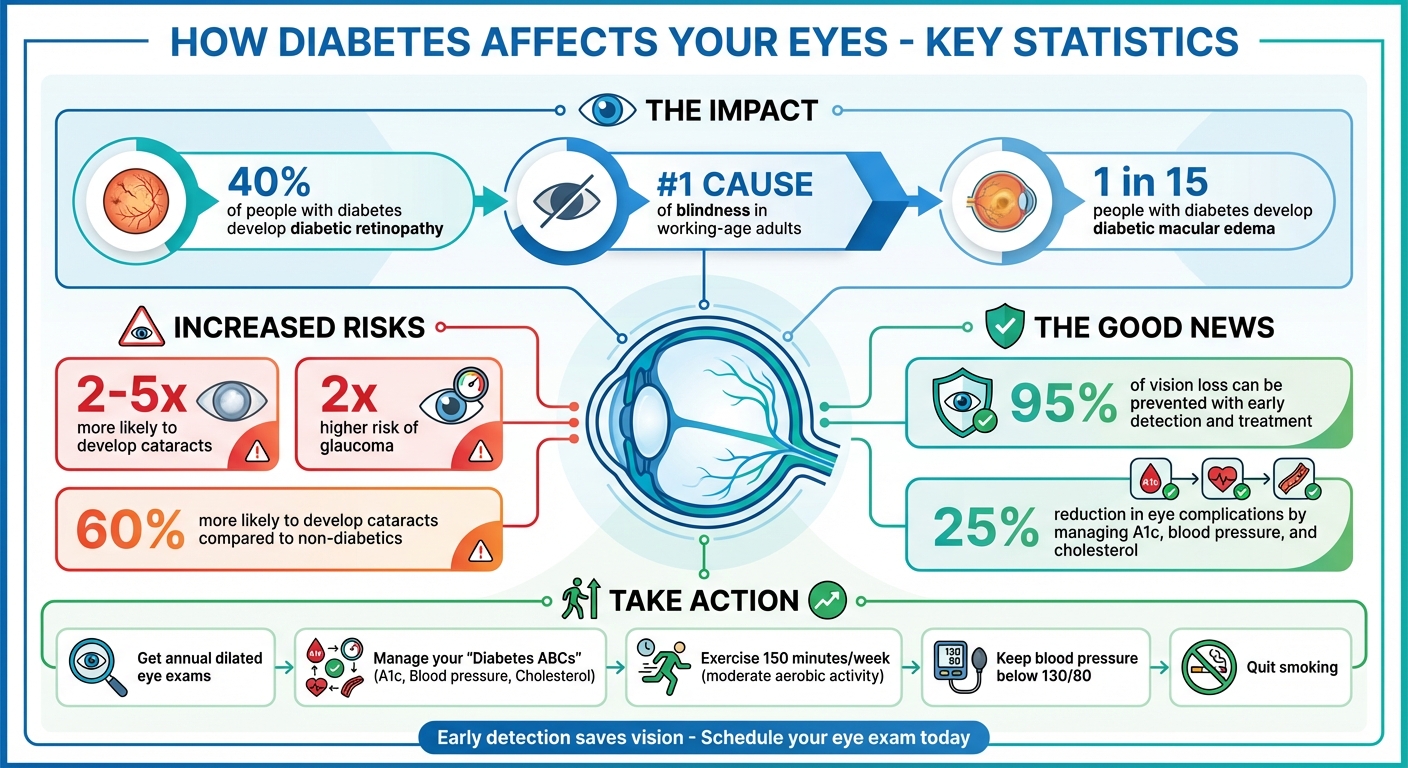
How Diabetes Affects Your Eyes: Key Statistics and Prevention Facts
How Diabetes Damages Your Eyes
How High Blood Sugar Harms Eye Tissue
When blood sugar levels remain elevated for extended periods, they can weaken the tiny blood vessels in your retina – the delicate tissue at the back of your eye. These weakened vessels may bulge and form microaneurysms, which can leak fluid and blood into the surrounding tissues.
"High glucose can change fluid levels or cause swelling in the tissues of your eyes that help you to focus, causing blurred vision."
As the damage progresses, blocked blood vessels deprive retinal tissue of oxygen. In response, the eye tries to compensate by growing new, fragile blood vessels. Unfortunately, these vessels often bleed into the vitreous – the gel-like substance inside your eye – leading to further complications. Additionally, fluid leakage into the macula, the central part of the retina, causes diabetic macular edema, a condition that affects about 1 in 15 people with diabetes.
High blood sugar also disrupts the eye’s natural fluid balance. For instance, fluctuating glucose levels can cause the lens to swell or change shape, leading to temporary focusing problems. Over time, sugar deposits may build up in the lens, causing it to cloud over – a condition known as cataracts. In severe cases, abnormal blood vessel growth on the iris can block the eye’s drainage system, increasing internal pressure. This condition, called neovascular glaucoma, can damage the optic nerve.
Why Diabetes Increases Your Risk of Vision Loss
The structural damage caused by diabetes creates a ripple effect throughout your visual system, significantly increasing your risk of vision problems. Diabetes doesn’t just affect one part of the eye; it makes the entire system more vulnerable. For example, people with diabetes are 2 to 5 times more likely to develop cataracts than those without the condition, and their risk of glaucoma is twice as high as the general population.
In addition to accelerating common age-related eye issues, diabetes can lead to specific complications. Diabetic retinopathy, for instance, is the leading cause of blindness among working-age adults. Nearly half of those with this condition eventually develop diabetic macular edema, further threatening their vision. Rita Rastogi Kalyani, M.D., M.H.S., a diabetes expert at Johns Hopkins, explains:
"Elevated blood sugar levels can damage blood vessels in the retina – the area at the back of the eye that sends signals to your brain. This damage, called diabetic retinopathy, can begin years before you notice vision changes."
The good news is that managing your "diabetes ABCs" – A1c (average blood sugar), blood pressure, and cholesterol – can significantly reduce the risk of microvascular complications, including those affecting your eyes, by as much as 25%.
Eye Conditions Caused by Diabetes
Diabetic Retinopathy: The Primary Threat
Diabetic retinopathy stands as the leading cause of blindness among working-age adults in the U.S. This condition progresses through stages, beginning with nonproliferative diabetic retinopathy (NPDR). In this early stage, the walls of the retinal blood vessels weaken, leading to the formation of microaneurysms. These tiny bulges can leak fluid or blood into the surrounding retinal tissue. Additionally, larger vessels may swell and become uneven in width.
As the disease advances to proliferative diabetic retinopathy (PDR), blocked blood vessels prompt the retina to grow fragile new ones. These vessels are prone to bleeding into the vitreous – the gel-like substance inside the eye – causing symptoms like floaters, dark streaks, or even a complete loss of vision.
Diabetic retinopathy affects about 40% of people with diabetes. A particularly concerning complication is diabetic macular edema (DME), which impacts roughly 1 in 15 individuals with diabetes. DME occurs when fluid leaks from damaged blood vessels, causing the macula – the part of the retina responsible for sharp, central vision – to swell. This swelling distorts vision, making tasks like reading or recognizing faces difficult.
These progressive changes emphasize the importance of timely treatment, but diabetic retinopathy isn’t the only eye condition linked to diabetes.
Other Eye Problems Linked to Diabetes
Diabetes can speed up cataract formation and nearly doubles the risk of developing glaucoma. A more severe form, neovascular glaucoma, occurs when abnormal blood vessels obstruct the eye’s drainage system. Other complications include vitreous hemorrhage, where fragile vessels bleed into the eye’s center, and tractional retinal detachment, a condition where scar tissue from abnormal vessel growth pulls the retina away from the back of the eye.
The good news? Early detection and treatment of diabetic retinopathy can lower the risk of blindness by 95%. Regular, comprehensive eye exams are crucial for catching these issues early. Identifying and addressing these complications underscores the critical role of routine eye care for individuals with diabetes.
Warning Signs of Diabetic Eye Disease
Symptoms to Watch For
In the early stages, diabetic eye disease often sneaks in without any noticeable symptoms. According to the National Institute of Diabetes and Digestive and Kidney Diseases, "Often, there are no warning signs of diabetic eye disease or vision loss when damage first develops". You could have perfect 20/20 vision while the blood vessels in your retina are silently undergoing damage.
When symptoms do appear, they might include blurry or wavy vision, dark spots or floaters, difficulty distinguishing colors, poor night vision, or trouble focusing on detailed tasks. These changes can sometimes be temporary, especially if they’re tied to fluctuating blood sugar levels. However, they might also signal more serious, lasting damage.
Certain symptoms require immediate medical attention. If you experience sudden flashes, an increase in floaters, or a dark "curtain" obscuring part of your vision, these could be signs of retinal detachment. Recognizing these warning signs highlights why regular eye check-ups are so important.
Why You Need Regular Eye Exams
Since diabetic eye disease can progress without noticeable symptoms, regular eye exams are crucial for catching problems early. Eye specialists can identify damage long before you experience any changes in your vision. A dilated eye exam is particularly important, as it allows doctors to thoroughly inspect your retina, blood vessels, and optic nerve – areas that a basic vision test won’t reveal.
If you’ve been diagnosed with Type 2 diabetes, schedule a dilated eye exam as soon as possible. For those with Type 1 diabetes, it’s recommended to have your first exam within five years of diagnosis, followed by annual check-ups. Pregnant women with diabetes should prioritize an exam early in their pregnancy, as diabetic retinopathy can worsen rapidly during this time.
The Centers for Disease Control and Prevention stresses the importance of early detection: "The sooner you’re treated for DR [diabetic retinopathy], the better that treatment will work. That’s why early diagnosis is so important, even if you don’t have symptoms yet".
For those in Denver, Colorado, Denver Eye Surgeons offers comprehensive diabetic eye care, including same-day appointments, ensuring you have access to specialized care when you need it most.
sbb-itb-929a4e2
How to Prevent and Manage Diabetic Vision Problems
Managing Blood Sugar and Making Lifestyle Changes
Diabetes can take a serious toll on your vision, but there are steps you can take to protect your eyes. It starts with managing the "Diabetes ABCs" – A1c (average blood sugar), blood pressure, and cholesterol levels. These three factors play a direct role in the health of the small blood vessels in your retina. By staying active, eating a balanced diet, and sticking to prescribed medications, you can help delay or even prevent vision loss.
Keeping your blood pressure below 130/80 is particularly important for protecting those delicate retinal blood vessels. Incorporate at least 150 minutes of moderate aerobic activity per week – even something as simple as a brisk walk can help. However, if you’ve already experienced diabetic eye damage, avoid activities like heavy weightlifting or high-impact exercises that could strain your eyes.
If you smoke, quitting is one of the best things you can do for your eye health. Smoking increases the risk of diabetic retinopathy and other complications. A well-rounded diet is also key – it helps stabilize your blood sugar and prevents sugar deposits from forming in the lenses of your eyes. These lifestyle adjustments create a strong foundation for managing your vision and may reduce the need for more intensive treatments.
Treatment Options and Specialized Care
When lifestyle changes aren’t enough, medical treatments step in to help. Anti-VEGF injections are a common option – they work by blocking proteins that trigger abnormal blood vessel growth in the retina, slowing or even reversing retinopathy. Another option, laser photocoagulation, seals leaking blood vessels and reduces swelling in the retina. For more advanced cases, vitrectomy surgery can remove scar tissue and cloudy fluid from the eye.
For diabetic macular edema, corticosteroid injections or implants can help reduce swelling in the retina. If cataracts develop – a condition that people with diabetes face about 60% more often – surgical lens replacement can restore clear vision. Glaucoma, another potential complication, is usually treated with specialized eye drops, laser therapy, or surgery to lower eye pressure.
Clinics like Denver Eye Surgeons provide comprehensive care for diabetes-related eye problems. They offer same-day appointments and advanced tools like fluorescein angiography and digital retinal imaging to diagnose and monitor conditions. Their team of skilled ophthalmologists performs procedures such as vitrectomies and retina injections, ensuring patients receive the precise care needed to protect and preserve their vision.
How Diabetes Affects Your Eyes & Vision : Understanding Signs & Symptoms
Conclusion: Protecting Your Vision from Diabetes
Diabetes doesn’t have to lead to vision loss. While it can harm the delicate blood vessels in your retina and increase the chances of cataracts and glaucoma, early intervention can lower the risk of blindness by a staggering 95%. The secret lies in addressing issues before symptoms even surface. By the time you notice changes in your vision, the damage may already be irreversible. That’s why early detection remains the foundation of effective diabetic eye care.
"Early detection gives you time for treatments, such as laser therapy, that can protect your eyes. It also gives you more time to protect your vision by controlling blood sugar and blood pressure." – Rita Rastogi Kalyani, M.D., M.H.S., Johns Hopkins diabetes expert
Getting a yearly dilated eye exam is non-negotiable. These exams enable your eye doctor to identify changes in blood vessels, swelling, or early signs of retinopathy before they pose a serious threat to your vision. Beyond these exams, keeping your A1c, blood pressure, and cholesterol levels in check can slash your risk of eye complications by 25%. Adopting healthier habits – like staying active, eating balanced meals, and quitting smoking – can also help protect those delicate retinal blood vessels from the effects of high blood sugar.
Taking a proactive stance is critical. Preventing vision loss from diabetes hinges on both prevention and timely treatment. Should you develop diabetic eye disease, modern treatments like anti-VEGF injections, laser therapy, or surgery can halt its progression and, in some cases, even restore lost vision. Clinics like Denver Eye Surgeons provide specialized diabetic eye care, equipped with advanced diagnostic tools and same-day appointments to safeguard your eye health. Whether you need routine monitoring or advanced treatment, their team is ready to help you preserve your sight.
Don’t wait – schedule your annual eye exam, manage your blood sugar, and seek care promptly. Protecting your vision starts with taking action today. Your eyes deserve the best care to prevent diabetes from casting a shadow over your future.
FAQs
What are the early signs of diabetic eye disease?
Diabetic eye disease, including diabetic retinopathy, can be sneaky. In its early stages, it often doesn’t come with any noticeable symptoms, making regular eye exams absolutely critical. But as the condition advances, you might start noticing things like:
- Floaters – those little spots or strings drifting across your vision
- Blurred or fluctuating vision
- Dark or empty areas in your visual field
- Gradual loss of vision
These changes tend to creep in over time, often without pain or any clear warning signs. That’s why scheduling annual dilated eye exams is so important – it’s your best chance to catch issues early and avoid serious vision problems. And if you do notice any changes in how you see, don’t wait to act. For those in Denver, Denver Eye Surgeons provides specialized diabetic eye care to help safeguard your sight.
How does controlling blood sugar levels help protect your vision?
Keeping your blood sugar in check plays a key role in safeguarding your vision. Elevated blood sugar levels can harm the delicate blood vessels in your retina, heightening the risk of conditions like diabetic retinopathy. Left untreated, this condition can lead to vision loss. By managing your glucose levels effectively, you not only protect your eyes but also promote better overall eye health.
For those living with diabetes, scheduling regular eye exams is equally important. These check-ups can catch potential problems early, making treatment more effective. Clinics like Denver Eye Surgeons specialize in diabetic eye care, offering the expertise needed to help you preserve your vision and avoid complications.
What are the treatment options for diabetic retinopathy?
Diabetic retinopathy treatments are designed to slow the condition’s progression and safeguard your vision. Some of the most common approaches include laser therapy, which helps seal leaking blood vessels and reduces swelling in the retina, as well as intravitreal injections. These injections often deliver medications like anti-VEGF agents, which work to control abnormal blood vessel growth and fluid buildup. For more severe cases, a vitrectomy might be necessary. This surgical procedure removes blood or scar tissue from inside the eye to restore clearer vision.
Keeping your blood sugar levels in check plays a key role in preventing further damage and minimizing the need for more invasive treatments. Regular eye exams are equally important – they enable early detection and timely treatment, which can make a big difference in preserving your eyesight. If you’re located in the Denver area, Denver Eye Surgeons provides specialized diabetic eye care to help protect and maintain your vision.
